By Category
By Type
By Author
-
How immense is farming’s problem with plastic?
-
Giving food a bad wrap: Why we need to stop relying on plastic
-
Preserving the practices of traditional foods
-
How our paranoia about contamination is threatening local food
-
The Puglia paradox: Why pest invasions and historically high prices could actually be good for olive oil
-
Roots to regeneration: Growing regenerative leadership in food and farming
-
Reviews: Food and farming in film 2024
-
Understanding the farmer protests
-
What is ‘local’ food and why does it matter?
-
For the love of Cawl
-
For the love of home-cooked food
-
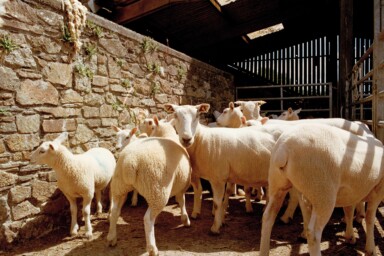
More than a by-product: Resetting the way we think about wool
-
Beans are good for people and the planet, so why aren’t we eating more of them?
-
Progress for local abattoirs at ORFC
-
Views from ORFC: Inspiration for food and farming in 2024
-
ORFC 2024: Highlights from this year's conference